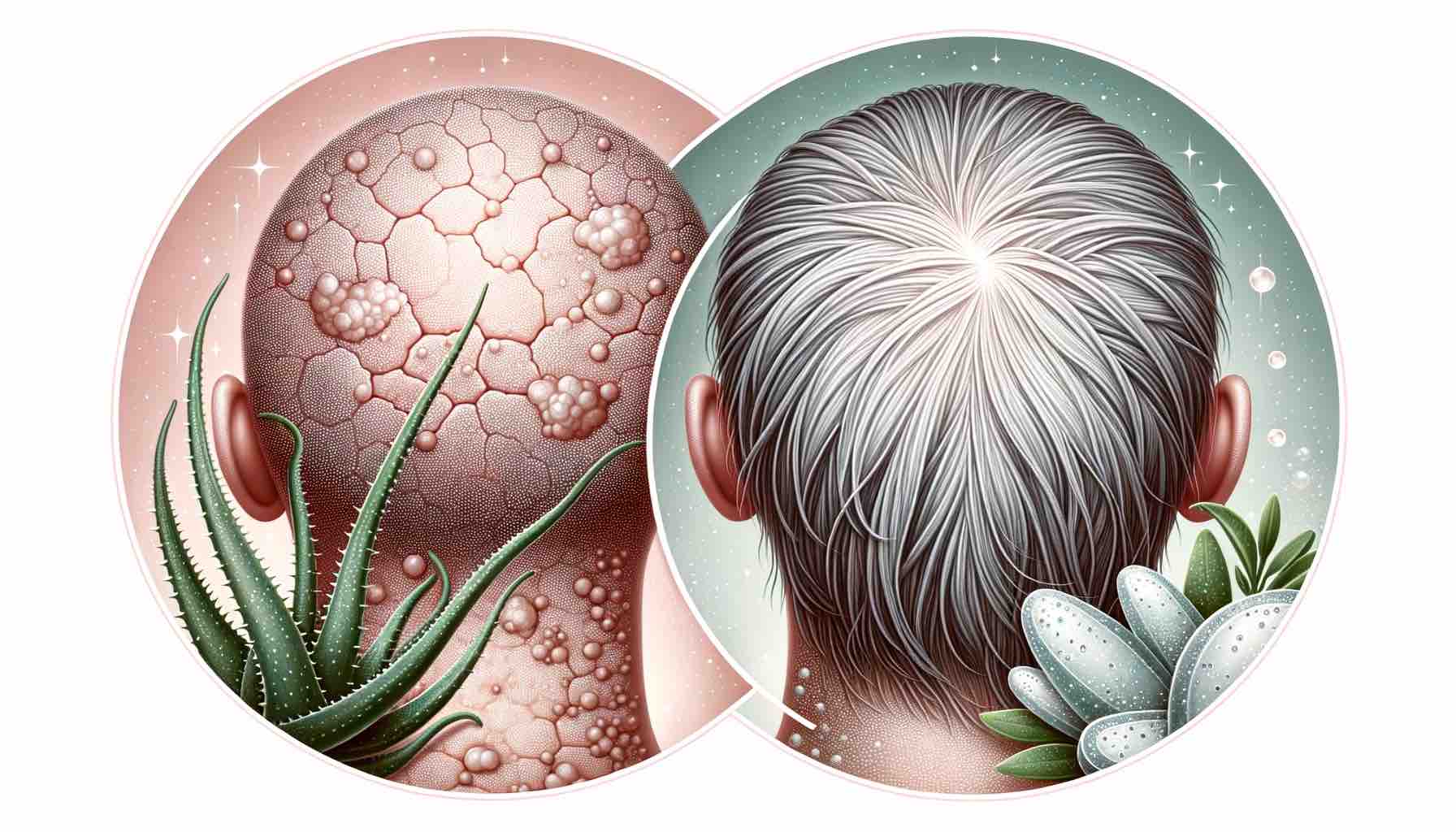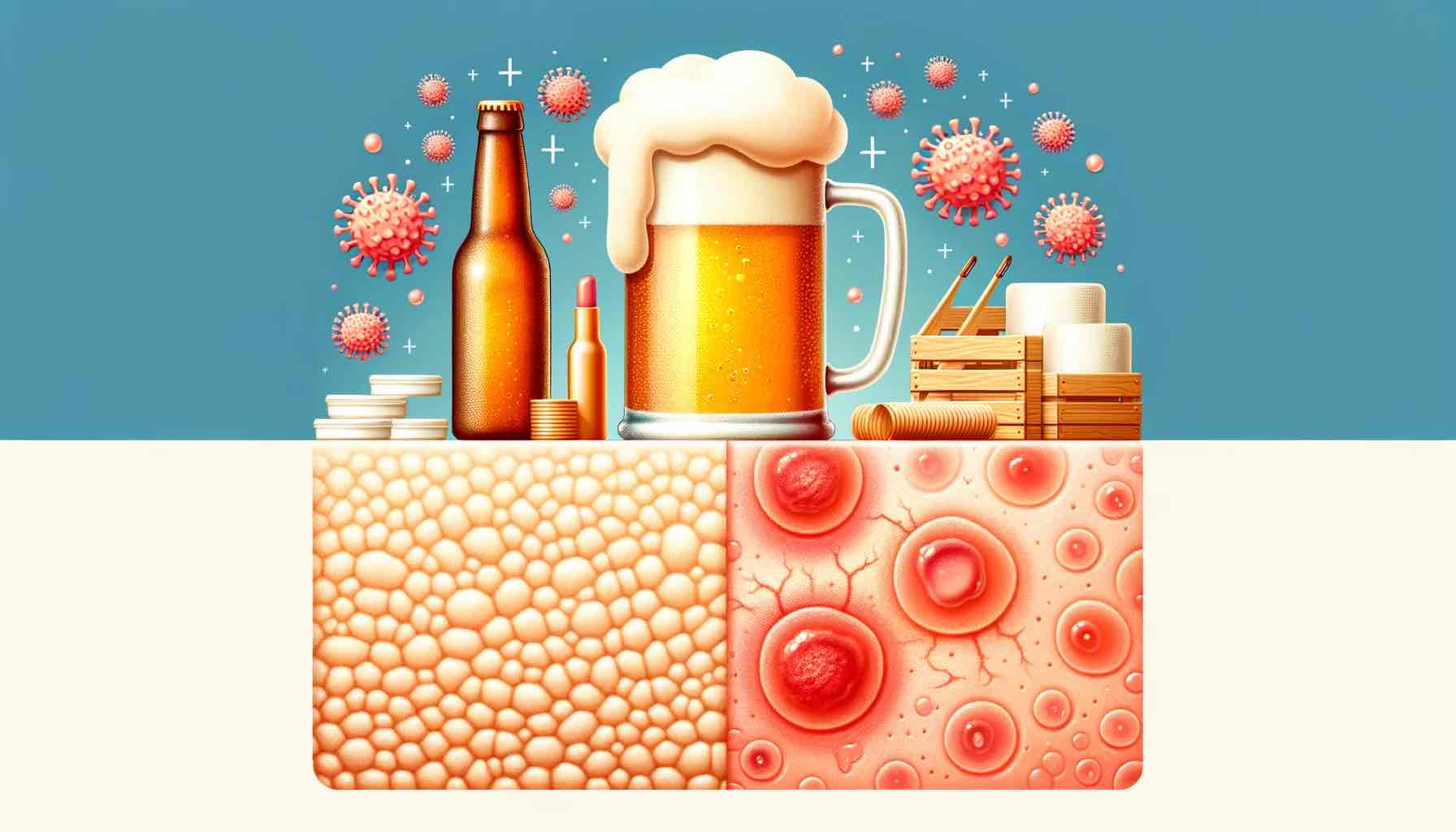
Eczema, a condition marked by inflamed, itchy, and red skin, can be influenced by various factors ranging from environmental triggers to dietary habits. One question that often surfaces is the role of alcoholic beverages, particularly beer, in managing eczema. Does beer consumption exacerbate the symptoms, or is it just a myth? In this article, we will unravel the relationship between beer and eczema, diving deep into scientific research, personal anecdotes, and practical insights.
Understanding Eczema: The Basics
Eczema, also known as dermatitis, is a skin condition characterized by patches of itchy, inflamed skin. Triggers can range from allergens, irritants, stress, climate, to certain foods and beverages. Understanding these triggers is crucial in managing the condition effectively. For more detailed insights into the condition, you might want to explore Food and Atopic Dermatitis or Eczema.
Beer and Its Components: What’s in the Bottle?
Beer is a popular alcoholic beverage consumed worldwide. But what does it contain that might influence eczema? Beer is a concoction of water, malted barley, hops, and yeast. Certain components, like yeast and gluten, are potential allergens that might impact individuals with eczema adversely.
Beer as a Potential Eczema Trigger: The Science
Alcohol, including beer, can influence the immune system and inflammatory responses in the body. It might also lead to dehydration, affecting the skin’s ability to heal and regenerate. Discussing the specifics, beer contains ingredients like yeast and gluten, known to be potential triggers for eczema flare-ups.
Scientific Backing: Research and Studies
While there is limited direct research on beer’s impact on eczema, studies on alcohol and skin conditions provide some insights. Alcohol consumption has been linked to increased inflammation, which could exacerbate eczema symptoms. However, the direct correlation between beer and eczema remains a subject requiring more comprehensive research.
Personal Experiences and Anecdotes: Varied Responses
People’s experiences with beer and eczema vary. Some find that beer consumption worsens their symptoms, while others do not notice a significant impact. It’s essential to consider these personal stories while also consulting healthcare professionals for personalized advice.
Practical Advice: Navigating Beer Consumption
If you have eczema, moderating beer consumption or opting for gluten-free or non-alcoholic versions might be worth considering. Observing your body’s response and discussing with a healthcare professional can guide your choices better.
Conclusion: A Personalized Approach
The relationship between beer and eczema is multifaceted. While certain components in beer might trigger eczema symptoms in some, the overall impact varies individually. A personalized approach, considering one’s own body responses and professional medical advice, is essential in navigating beer consumption for those with eczema.
Further Reading and Resources
For a broader perspective on diet and eczema, exploring articles like Fruits and Eczema can be quite enlightening, offering various viewpoints and comprehensive insights.
FAQs
- What components in beer might trigger eczema symptoms? Beer contains ingredients like yeast and gluten, which are known allergens that might exacerbate eczema symptoms in some individuals.
- How does alcohol consumption generally affect eczema? Alcohol can influence the immune system and inflammatory responses, potentially leading to increased eczema flare-ups and skin sensitivity.
- Are there specific types of beer that are more likely to cause eczema flare-ups? Beers containing higher amounts of gluten and yeast, or those with a higher alcohol content, might be more likely to influence eczema symptoms.
- Is it possible to consume beer without worsening my eczema symptoms? It varies from person to person. Some might find relief by choosing gluten-free beers or moderating their consumption, but it’s essential to observe personal reactions and consult a healthcare professional.
- How can I determine if beer is a trigger for my eczema? Keeping a food and symptom diary, noting any flare-ups correlated with beer consumption, can be a helpful way to identify if beer is a trigger for your eczema.
- Can non-alcoholic beer also affect eczema? Non-alcoholic beer might be a better option due to lower alcohol content, but it still contains potential allergens like gluten and yeast that could affect eczema.
- What are some alternatives to beer for individuals with eczema? Exploring beverages that do not contain common allergens found in beer, such as gluten-free or non-alcoholic options, might be worth considering.
- Does the frequency of beer consumption impact eczema symptoms? Frequent consumption might increase the likelihood of flare-ups, but individual tolerance levels vary, making it essential to observe personal reactions.
- Are there any studies that directly link beer consumption to eczema flare-ups? Direct research specifically linking beer to eczema is limited, but studies on alcohol and skin health provide insights into potential connections.
- Where can I find more information on diet and eczema? Various resources, like Food and Atopic Dermatitis or Eczema, offer comprehensive insights into the relationship between diet and eczema.
Blog Tags
eczema, beer, dermatitis, skin health, alcohol and skin, eczema triggers, dietary influences on eczema, gluten, yeast